WHERE CAN RENEWAL INFORMATION FOR BLUE PLUS MEMBERS BE FOUND?
- Full Detail & New Cap enrollment reports.
- Renewal Roster report.
- Posted in Bridgeview around the 25th of every month (date varies month-to-month).
- Made up of members whom DHS is reporting are due to complete their MA renewal within 45 days or less of the report.
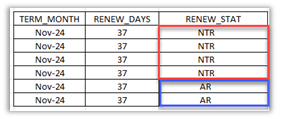
- TERM_MONTH indicates the date that the member will procedurally term if member renewal is not received/processed by the first of the month listed. In the example below, potential procedural term date is NOV 1.
- RENEW_STAT codes indicate a member’s renewal status.
- NTR – Need to Renew
- AR – Auto-renewed
WHAT CARE COORDINATORS SHOULD DO
- If you are aware that a member’s address has changed, report to County/Tribal worker via DHS-8354 – MCO Member Address Change Report Form.
- If a member has a change in living arrangement – I.E. from community to nursing facility or vice versa, continue reporting to County/Tribal worker using form DHS-5181.
- Review Blue Plus enrollment reports for upcoming or past-due MA Renewal dates, as reported by DHS.
- Utilize the monthly Renewal Roster to conduct required outreach for members flagged as NTR – Need to Renew.
- Outreach can be to member/AREP and/or to County/Tribal worker and must be completed by the 15th of the following month.
- Example: Renewal Roster posts 9/25, outreach should be completed by 10/15.
- Outreach can be completed by Care Coordinators or Admin staff.
- Delegates may find it easier/more convenient to reach out to County/Tribal worker, and reach out to members only as necessary.
- Please note: If County/Tribal worker states they are unable to give you information or discuss a member’s MA renewal, please email the details of interaction, person you spoke with, and how to partner.relations@bluecrossmn.com for follow-up.
DHS RENEWAL RESOURCES FOR USE BY CARE COORDINATORS
- MCO Member Address Change Report Form – Address updates only – not for use when reporting a change to member’s living arrangement (I.E. NH to COMM).
- DHS-5181 – Used to report changes such as member living arrangements (I.E. COMM to NH)
- Renewal Look-up Tool
- Renewal Upload Tool
- Renewal forms
- County or Tribal Directory
- Medical Assistance and MinnesotaCare info
- Income and Asset Limits
- Renewing MA and MinnesotaCare Eligibility
GENERAL ELIGIBILITY REMINDERS:
- A member’s renewal date will depend upon their initial application date.
- Around 6 weeks (45 days) before their renewal is due, DHS will mail out applicable information.
Example: If a recipient initially applied for MA in July, renewal information will be mailed to them in May.
- If a County or Tribal worker can automatically renew a recipient’s MA:
- The member will receive an auto-renewal notice, along with a summary of information used to make this determination. Members are instructed to review, and are advised that if everything is correct, no action is needed.
- If any information used to auto-renew is incorrect/requires updating, the member must contact their County or Tribal financial/income maintenance worker to discuss.
- If a County or Tribal worker cannot automatically renew a recipient’s MA:
- The member will receive a renewal packet with a form to complete, sign and return. If the cover letter/return envelope is lost, Care Coordination staff can provide County/Tribal mailing address or members can be directed to contact their County/Tribal worker.
- Renewal application & proofs can also be conveniently and quickly submitted online or with a smart phone by using DHS’s Renewal Upload Tool. Care Coordination staff can also submit documents using the upload tool, on behalf of the member.
- Including proof of income/assets with the renewal form may help County/Tribal worker process the renewal more quickly. Example of proofs include but are not limited to:
- Current checking/savings bank statement
- Proof of ownership for stocks, bonds, savings certificates, trust funds or other financial assets
- Proof of current unearned income
- Pay stubs if applicable
- Life insurance policies
- Income/asset limits depend upon the program and may be reduced (spent down) to maintain eligibility. For additional info, please consult with a County/Tribal worker or review DHS info.
- Renewal info should be returned as soon as possible to allow County/Tribal workers time to process and to avoid a potential break in service.
- Lengthy processing times are anticipated.
- If renewal is past due and coverage has ended, members should still be encouraged to return so that a County/Tribal worker can evaluate eligibility for an official determination.
- If renewal and proofs are received before the last day of the fourth month following closure, County/Tribal workers can still evaluate eligibility using the completed renewal document and proofs, if applicable. If returned after that, member will need to reapply.
